
Have you ever heard that your gut is your second brain? Scientists are linking our overall health including digestive, mental and physical health to our gut or more specifically, our microbiome.
What is microbiome? The microbiome is the genetic material of all the microbes - bacteria, fungi, protozoa and viruses - that live on and inside the human body. The number of genes in all the microbes in one person's microbiome is 200 times the number of genes in the human genome. The microbiome may weigh as much as five pounds, which is about the same as our brains.

Digestive system problems such as heartburn, gas, bloating and constipation, and diarrhea reflect what’s happening throughout your body. The main drivers of gut health change are shifts in stomach acid, gut immunity and gastrointestinal flora—the complex ecosystem of bacteria in your digestive system and microbiome. Our microbiome
- Protects us against germs
- Breaks down food to release energy
- Produces vitamins
- Produces precursors to neurotransmitters and hormones
When gut health is good, your physical and mental health tend to follow. When gut health is poor it can lead to anxiety, depression, and weight gain. This article will look at those two facets of gut health.
Mental Health
It used to be thought that metal health disorders are a chemical imbalance in the brain or a disease brought on by genetics, traumatic experience, or hereditary. In certain cases this may very well be true however numerous studies have shown a strong link to an unhealthy gut and an increase in anxiety & depression.

To reference a study published in Pub Med "A growing body of literature supports and characterizes a gut-brain axis, and elucidates a possible role of gut microbiome dysfunction in major depression. Associations between the gut microbiome and depression have been identified in studies of inflammatory states and gut barrier health (17–19)
Let’s examine what causes poor gut health and how that can trigger lack of motivation, anxiety and depression.
Cytokines are proteins that are produced by cells and regulate inflammation. Cytokines interact with cells of the immune system in order to regulate the body's response to disease and infection, as well as mediate normal cellular processes in the body. There are pro- inflammatory and anti-inflammatory cytokines.
When pro inflammatory cytokines are chronically elevated serotonin is not produced at normal levels in the body (serotonin is a precursor to dopamine which is our bodies happy drug) Serotonin is suppressed because the body links chronic inflammation to disease. When in a state of disease moving/energy expenditure is not the bodies priority. Generally, when dopamine is elevated we are moving, social, happy and enjoying life. Low dopamine, low energy.
When pro inflammatory cytokines are elevated, we also want to put LESS energy and effort into obtaining food which may drive us to “order out” or go for food choices that require very little energy and motivation to prepare.
To sum it up, chronic inflammation in the gut, causes our body to think it is in a state of disease which reduces Serotonin production which in term both decreases our desire to move or lowers energy but also reduces dopamine production. Think of it this way, if you have ever gone on a refreshing walk or endured a great workout you generally feel great afterward. This is from the dopamine release. When serotonin is low, we forget or “discount” how good it fells to workout or move. We might just want to lay on the coach or sleep. Scientists call this EFFORT DISCOUNTING. We simply do not believe that the activity that will release our feel-good chemical, dopamine, is worth doing. It is also important to note that l-tryptophan is a precursor to serotonin. When the microbiome is unbalanced tryptophan is chemically broken down to a bi product called kynurenine. Elevated levels of kynurenine are associated with anxiety, depression and Alzheimer’s
Notice that the start of this entire cascade or process in an unhealthy gut caused by inflammation! The inflammation comes from what we are feeding our microbiome Inflammatory foods kill our good bacteria and allow the bad bacteria to feed and become predominant. Ever feel like lying on the coach all day after a night of drinking, greasy foods, low sleep and absence of anti-inflammatory foods? The lack of motivation stemmed from inflammation in the gut caused by those activities.
Now it is not a far stretch at all to see how if our motivation, mindset, and energy are brought down from an unhealthy gut then weight gain is almost a sure thing. Unfortunately, from a weight loss and gain perspective there is a bit more to it other than the serotonin/dopamine/energy loop.
Chronic low-grade inflammation can take 30% of our total calories needed per day making us feel very lethargic and slow us down. 40% of our total energy expended in a day is movement based. If 30% of our total energy is being used to deal with chronic inflammation then we are not going to move with as much vigor, energy, and as much thus burning less calories per day. Think of when you are sick and your body is fighting a cold you tend to rest and move less.
Chronic inflammation is keeping our body in a constant state of “rest”
Weight gain is associated with different profiles of gut health with the primary one researched being the ration of firmicutes and Bacteroidetes. Firmicutes are shown to be a type of bacteria that is efficient at extracting calories from food. Thus, if we are eating more then these “fat bugs” are helping us absorb more of those calories than we would if our gut was in balance.
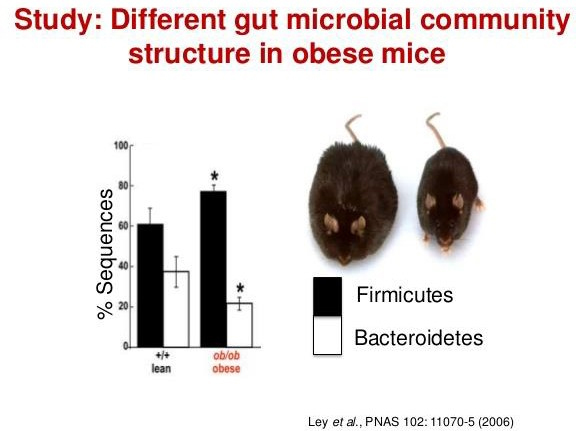
To quote another PubMed study “A possible explanation for our findings is that Firmicutes are more effective as an energy source than Bacteroidetes, thus promoting more efficient absorption of calories and subsequent weight gain [5,6]. In a study by Turnbaugh et al. [27] conducted in obese and lean twins, it has been shown that Firmicutes were dominant in the microbiomes of obese subjects, which were also enriched with genes known to be associated with nutrient transporters, while a higher relative abundance of Bacteroidetes and an enrichment of genes linked to carbohydrate metabolism was found in microbiomes of lean twins.”
Can you guess which type of foods firmicutes thrive on? You guessed it, highly processed foods that increase inflammation.
Now that we understand the importance of keeping our second brain healthy and how inflammation affects our gut health then lets look at how we can reduce inflammation, especially in the gut. We have done an entire article on how to reduce inflammation in the entire body so here we will focus on reducing gut inflammation.
- Eat more high-fiber foods. High-fiber foods such as legumes, beans, peas, oats, bananas, berries, asparagus, and leeks have shown a positive impact on gut health.
- Garlic and onion can be very gut healthy
- Fermented foods such as kombucha
- Collagen-boosting foods
We hope that this helps build your awareness and take action on improving your gut and overall health! For a more complete list of foods that damage your gut and foods that help it email us at coaching@macromissionary.com or message us on FB @macromissionary or IG @macro_missionary_
